Urticaria or also known as hives
Def : hives are raised, often itchy, red welts on the surface of the skin. They are usually an allergic reaction to food or medicine
Causes:
allergic reaction to a substance- your body releases histamine and other chemicals into your bloodstream.- itching, swelling, and other symptoms.
When swelling or welts occur around the face, especially the lips and eyes, it is called angioedema. Swelling from angioedema can also occur around your hands, feet, and throat
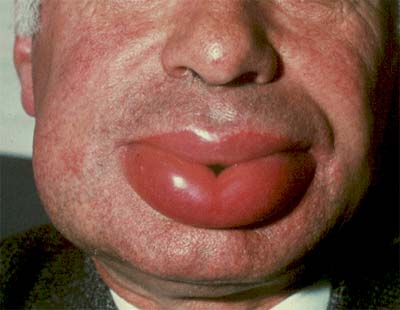
angioedema
Many substances can trigger hives, including:
- Animal dander (especially cats)
- Insect bites
- Medications
- Pollen
- Shellfish, fish, nuts, eggs, milk, and other foods
Hives may also develop as a result of:
- Emotional stress
- Extreme cold or sun exposure
- Excessive perspiration
- Illness (including lupus, other autoimmune diseases, and leukemia,hepatitis B
- Infections such as mononucleosis
Treatment
Treatment may not be needed if the hives are mild. They may disappear on their own. To reduce itching and swelling:
- Avoid hot baths or showers.
- Avoid irritating the area with tight-fitting clothing.
- Take antihistamines. Diphenhydramine is considered the most effective.
If your reaction is severe, especially if the swelling involves your throat, you may require an emergency shot of epinephrine (adrenaline) or steroids. Hives in the throat can block your airway, making it difficult to breathe.
.













